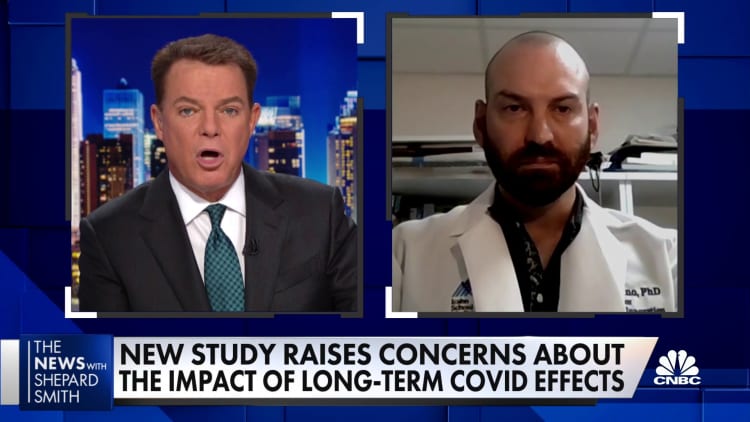
Long Covid costs patients an average of $9,000 a year in medical expenses

The Covid-19 unit at United Memorial Medical Center north of Houston.
Carolyn Cole | Los Angeles Times | beautiful pictures
The Covid-19 Pandemic has so far affected 23 million Americans — and it’s poised to have a financial impact that equals or exceeds that of the Great Recession. According to one estimate, chronic disease will cost the US economy $3.7 trillionwith additional medical costs accounting for $528 billion.
Costs at household and national scales are difficult to quantify because the disease – also known as persistent, post-Covid or post-acute Covid syndrome – is so new. Anyone who has been infected with Covid-19 is susceptible to the disease, regardless of factors such as age, health or vaccine status.
Symptoms, which can number in the hundreds, can range from mild to severe and can last for months or even years.
David Cutler, an economist at Harvard University who has predicted the $3.7 trillion economic cost of prolonged Covid, estimate The individual medical costs of the illness averaged about $9,000 a year. However, typical costs can range from about $3,700 to nearly $14,000, Cutler said.
The cost can be much higher, depending on the severity of the disease. And because symptoms often affect a person’s ability to work, a person with persistent Covid may not rely on regular wages – or employer-sponsored health insurance – to help. cover those medical bills.
Cutler’s financial estimates are based on research to treat encephalomyelitis, a condition also known as chronic fatigue syndrome, or ME/CFS.
Dr. Greg Vanichkachorn, medical director of the Mayo Clinic’s Covid Active Recovery Program, said those estimates are the best current estimates, as treatment and assessment for long-term Covid also same as for ME/CFS. Have there is no approved cure or treatment for ME/CFS; As with prolonged Covid, the patient’s symptoms were only treated or controlled.
“I think it’s important to note that this is just an estimate,” Vanichkachorn said. “As new treatments come out, things can become more expensive or hopefully more affordable.”
“That’s the essence of the word ‘long distance’ – it can be an open cost box for a while,” says Vanichkachorn.
‘People are trying all kinds of treatments’
Obtaining an official long-term Covid diagnosis can be challenging, which can increase initial costs.
For example, those affected may undergo a series of tests to rule out other diseases. Or doctors can refer patients to specialists for treatment if they are unfamiliar with prolonged Covid or don’t want to consider it a possibility.
Medical professionals often treat infectious disease by identifying the invasive organism and attacking it. But that’s not what’s happening with prolonged Covid.

Instead, doctors treat the symptoms of the disease, not the disease itself, said Dr. Jeff Parsonnet, an infectious disease physician who started the Post-Acute Covid-19 Syndrome clinic at Dartmouth Hitchcock Medical Center, said.
Some of the most common lingering Covid symptoms include fatigue, post-exercise discomfort, chronic pain, cognitive dysfunction (also known as “brain fog”), concussion, and depression. , anxiety and heart or lung failure, follow for the United States Department of Health and Human Services. HHS says Long Covid can also cause other chronic conditions such as diabetes, encephalitis or chronic fatigue syndrome and heart disease.
Treatment is more about symptom control: If the patient feels tired, the doctor may recommend physical therapy; pain, take painkillers; if brain fog, possibly speech or occupational therapy; if depressed or insomniac, sleep studies, counseling, or psychiatric evaluation may be available.
“The real difficulty in treating patients with prolonged Covid is that we don’t know what causes it,” Parsonnet said. “People are trying all sorts of treatments, but that’s just conjecture at this point.
“They don’t cure anything, but they help people cope better,” he said, describing the treatments as “laborious and expensive.”
Health insurance is essential – if you can get it
Health insurance may cover some or most of the costs associated with diagnosis and treatment — that is, for people who have the disease.
Here’s what it looks like for three long-term Covid patients:
Uninsured professional visits and rent considerations
Rosa Santana
Source: Julia Santana
Rosa Santana, 56, is a self-employed yoga instructor in south Florida. She has no health insurance, so she is unable to see a specialist, although she feels like she is “living in a different body” since contracting Covid-19 in May 2020.
“Every time I go somewhere, I know it’s going to be $300 or $400, and [I wonder]’Will I pay the rent?'” Santana said of the doctor visits.
Yoga used to be a form of wellness for her. Now, it doesn’t bring the same relief as it used to; planting banana trees can make your heart beat faster and dizzy for days afterward.
The prolonged pandemic has affected Santana’s ability to work and her source of income to cover all her medical bills. Before, she was like the “energy bunny”; Now, she schedules two private yoga sessions with clients, and it’s time to “take a break,” she says.
Reach your annual out-of-pocket maximum with just one infusion
Donna Pohl
Source: Donna Pohl
Donna Pohl reaches her annual out-of-pocket maximum — about $3,500 — after just one infusion for common variable immunodeficiencyor CVID.
Pohl, 56, was healthy before a severe case of Covid that she was hospitalized in the fall of 2021. Now, CVID – a complication of prolonged Covid – puts her at higher risk of infection. Without insurance, Pohl would pay more than $10,000 per infusion; she needs them every month.
Pohl, who lives in Bettendorf, Iowa, has a team of 10 doctors, including one primary care physician and nine specialists.
In early 2022, she was diagnosed with Mast cell activation syndrome, a disease that causes a severe allergic reaction. She got pneumonia three times in one year. Pohl falls are often caused by “neuropathy,” a type of nerve damage; She ruptured a ligament in her left hand in a recent fall and required surgery to repair it.
“I’ve had a year out and I’m still having new symptoms,” she said.
Pohl, a practicing nurse at a hospital, considers herself lucky in a sense: She can’t be on duty in her grueling emergency room right now, but the hospital stays open. her (and employer-sponsored health insurance).
It’s been a year and I still have new symptoms
Donna Pohl
nurse practitioner
Without insurance, the cost of Pohl’s 156 medical claims through October of this year would amount to more than $114,000, records show.
Like many people with prolonged Covid, Pohl sought to alleviate the symptoms of paralysis wherever available.
That means she pays an average of about $300 to $400 a month for a variety of supplements and therapies that aren’t covered by insurance: chiropractic work, nutritional counseling, and hyperbaric oxygen, so far. “is the best treatment,” she says.
She lives on 60% of her previous income from a long-term disability policy – in a best-case scenario, the policy will continue until early 2024.
COBRA insurance and $4,000 deductible
Sam Norpel and her family. Norpel, 48, second from right, contracted Covid-19 in December 2021 and has not recovered. This chronic illness, known as persistent Covid, affects 23 million Americans.
Kirstie Donohue
Sam Norpel, 48, lost his job in June. The debilitating symptoms — including unpredictable slurs, cognitive problems, chronic fatigue, and severe migraines with prolonged screen viewing — prompted the former commercial executive Electronic cannot continue to work.
Norpel, who lives outside of Philadelphia, was able to negotiate for her employer to pay her lương COBRA premium for a year so she can keep her employer-sponsored health insurance.
Even with the health plan, the family paid about $4,000 out-of-pocket to hit the plan’s annual deductible. Norpel’s husband, who has quit his job to care for their children, is planning to return to the workforce in part to avoid losing his health insurance at work.
‘People… cured’ but it’s hard to see a specialist
There are nearly 250 cases after Covid clinic in the United States, according to Survivor Corps data as of early November. (A provider with multiple physical clinics counts only once.) The list is growing steadily: There were 178 in January.
Even so, According to the US Department of Health and Human Services, the spike in demand for specialists for prolonged Covid treatment means that sufferers can take up to a year to wait for an appointment.
Norpel contacted the Mayo Clinic in April, but the next consultation was about four months later, in August.
That’s the essence of the word ‘long distance’ – it can be an open cost box for a while.
Dr. Greg Vanichkachorn
medical director of Mayo Clinic’s Covid Active Recovery Program
Another hitch: She also has to pay to get there — a hotel room for a week and a round-trip plane ticket from Pennsylvania to Minnesota. She also couldn’t get a follow-up appointment with her neurologist until next February.
“A lot of us now take months to see specialists,” she said of longtime Covid patients.
However, when it comes to treatment, time is of the essence. Vanichkachorn said early intervention – usually less than four months from infection – has resulted in better outcomes for patients.
“Despite all the doom and gloom out there, people are actually getting better,” he said.
Patients at his clinic usually return to basic, normal activities four to six months after starting treatment, he explained.
Time alone often does not cure lingering Covid symptoms; it usually requires some form of rehabilitation. Months of inactivity can lead to severe physical impairment, adding to the patient’s discomfort. Physical and occupational rehabilitation helps strengthen muscles and helps patients reorganize their daily lives as they recover, says Vanichkachorn.
“People are really sick of being sick,” he said. “They try to push themselves too hard. “It’s hard to tell people we have to go slower, and that’s the only way we can help you get better as quickly as possible.”
Treatment delays can also have broader financial implications. HHS says patients are more likely to be denied financial assistance from disability insurance without a diagnosis and certification from professionals. They may also face more challenges when it comes to requesting workplace accommodation.
Despite the slow progress, patients and medical professionals remain optimistic. The US government has more than 72 active agencies Long-term Covid research program in place, according to HHS. One of them, the RECOVER initiative, led by the National Institutes of Health, has about 7,000 patients enrolled in clinical settings. CDC’s innovative support for patients infected with SARS-CoV-2 (or, INSPIRE) is enrolling 6,000 adults.
“The scale of Covid’s persistent morbidity and the breadth of its clinical manifestations represent an unprecedented, but not insurmountable, challenge,” according to HHS. Extended national COVID research action plan.
Vanichkachorn said the research is still in its early stages.
“We can have a completely new regimen two months from now, and people can recover suddenly,” he said.