An HR expert shows how telemedicine is stepping in to fill staffing shortages

Staff shortages are a major challenge in healthcare today. Another challenge is to find a solution to this annoying problem.
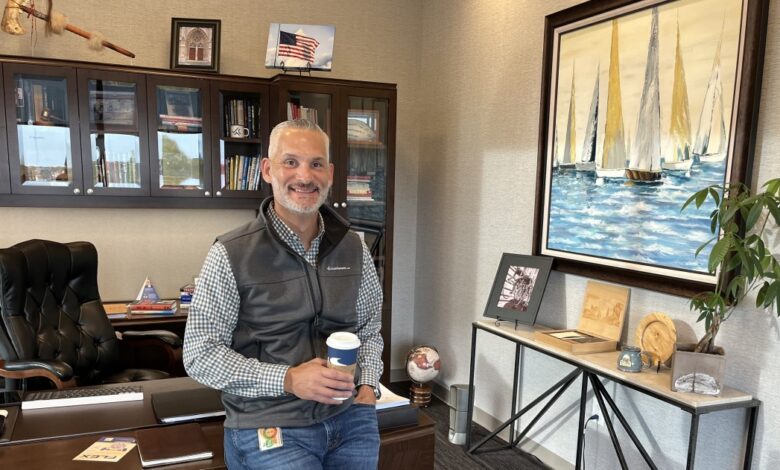
But Chris Franklin, president of LocumTenens.com, a self-service job board and full-service physician and cutting-edge practice recruitment agency working in the high-demand field, thinks telehealth has is becoming an emerging strategy to help fill gaps in hospitals and health systems. medical specialties.
Healthcare IT News sat down with Franklin to discuss the changes happening in the healthcare workforce, what he calls a hybrid HR strategy, and the results of a new survey by LocumTenens.com.
Q. Overall, what changes do you see happening in the healthcare workforce?
ONE. The changes we’ve seen in the broader economy regarding casual employment over the past three years have had an enormous impact on healthcare workers. There are a few key numbers that tell the story.
Current There are 3.5 million fewer workers in the US than there were two years ago. Since February 2020, job openings have increased by 50%, while total employment in the US has decreased slightly. Because demand is outstripping existing supply, workers are not only demanding higher wages, but also have more choice and control over when, how and where they work. This is especially true in healthcare, based on every metric we track.
New data shows More than 300,000 healthcare workers have left the workforce in the past two years. Doctors say they are choosing to retire early or leave full-time medical practice for other types of work, within and outside of our industry.
Frontline nurses have made the news because of the hardships they’ve been through, and also because of the freedoms they’ve been experiencing due to the rise in nursing travel. According to a 2021 study from According to the Department of Health, nearly 100,000 nurses left their jobs last year – most of them under the age of 50.
Again 32% of nurses said they could leave the profession. The Bureau of Labor Statistics estimates we will need to employ nearly 200,000 nurses each year through 2030.
Patient is sicker than ever. Over the past year, nearly every hospital has seen an increase in patient severity, largely due to delayed care during treatment. [COVID-19] epidemic. And chronic disease and obesity continue to be key drivers of healthcare consumption in the United States
Although it has been around for many years, the impact of a large population aging in the baby boom generation – The oldest person this year is 75 years old – finally here, and as a result the demand for healthcare is about to increase dramatically.
Burnout is also at an all-time high. One A recent survey from the MGMA and Jackson Physician Search highlights a pair of sobering statistics: Nearly two-thirds of physicians (65%) report they are experiencing burnout by 2022, up 4 percentage points. compared with the 2021 study. Among those with burnout, more than a third of doctors (35%) said their level of burnout increased significantly by 2022.
All of this points to a major shift across the industry and we are seeing first-hand that traditional workforce layout models no longer work, especially in health care field.
What is emerging is something very different – hybrid models predict both permanent and temporary employees, the proliferation of models that combine on-site care with strong presence strength of telehealth, the overall increase in APP staffing, and in general an increasing commitment to providing service providers with access to the kind of work-life balance that they are searching desperately.
Q. You say you’re seeing a hybrid HR strategy that includes elements of local tenants, more advanced practice providers, and more telehealth coverage . Please explain about this.
ONE. Healthcare leaders are looking for new and innovative solutions like never before – and all in the face of this healthcare workforce shortage.
We’ve seen firsthand the direct impact of the gig economy on the healthcare workforce, and know the biggest concern for healthcare facilities is attracting talent, retain talent, and avoid or minimize burnout.
To help clinicians eager to achieve a more viable work-life balance, healthcare leaders are evolving their hiring models to reflect a new appreciation about the flexibility that hybrid HR models exhibit. Relying solely on traditional HR models and solutions will no longer work. Through staffing innovation, hospitals and healthcare organizations are actively looking for options to improve access to care using more sustainable models.
Healthcare HR is complex and there is never a one-size-fits-all solution, but we are seeing growing interest in alternative staffing models, including increasing use of on-site tenants and improving patient access to care with advanced practice providers (APPs) and expanding care. remote healthcare.
Local tenant awareness and interest is at an all-time high for both healthcare organizations and clinicians. People are really taking their own health into account when working, choosing to do random work as a way to manage their stress and burnout levels.
We had an area physician tell the audience at a recent conference, “If you have regional burnout, you’re not doing it right.” Undoubtedly, the versatility of locum subscriptions offers a desirable outcome towards what doctors want out of life.
According to a recent survey:
- Nearly 90% of healthcare facilities already employ on-site staff.
- Nearly 57% of facilities that have not previously employed site staff are planning to use it in the next year.
Based on According to a recent survey we conducted on innovation and flexibility in staffing, when most administrators consider hiring on-site staff, they usually think about taking care of employees. on-site physician care. Data shows that hospitals use on-site tenants three times more often than telehealth, but that is starting to change.
Facilities that were previously dependent on on-site are now adopting telehealth. COVID-19 has accelerated this adoption, as hospitals have moved beyond traditional models to meet patient needs. In some cases, hospitals are adopting a flexible, hybrid approach that integrates telehealth and on-site care, bringing the best of both worlds and delivering value to patients. patient.
In addition, the use of APP in conjunction with doctors as a strategy is increasing, with 73.9% answering affirmatively to the question: “Do you have plans to expand the coverage of the APP?”
Q. Your company recently conducted a survey of hospital managers to gain insight into the challenges in today’s landscape. What have you learned as it relates to telehealth?
ONE. The results of our recent survey – detailed in the Report Innovation & Flexibility: A Journey towards Sustainable Health Care – show that hospital managers have strong responses when deals with managing today’s challenging landscape.
Regarding how it relates to telehealth, more facilities are using telehealth than ever before. COVID-19 has accelerated this adoption, but over the next year most hospitals are expected to expand their use of telehealth even further – there is no way back.
Patients across the board are now more comfortable using telehealth as the COVID-19 pandemic has led to a spike in virtual visits, including those who were previously hesitant use technology. Psychiatric services have traditionally dominated local telehealth services, with behavioral health accounting for 79% of telehealth services for LocumTenens.com.
However, usage has begun to change as hospitals consider other specialties, including oncology, cardiology, and physiology. By expanding telehealth services, facilities can expand access to care and reach more patients in new locations.
Over the past year, many facilities have been able to provide a higher level of intensive care to satellite or remote locations through telehealth. In the future, better matching reimbursements to the level of care provided in a telehealth setting will lead to wider adoption.
Q. Where do you see the telehealth component of employees in the next 5 years?
ONE. The feedback we received shows that more than half (60%) of those surveyed have plans to expand telehealth. Through innovation, healthcare providers will continue to adapt to flexibility and improve access to care. These flexible solutions create a more sustainable model for delivering quality care to patients and their communities.
Since clinicians are very concerned about patients receiving quality health care in a timely manner, I see telehealth programs as key to improving my outcomes. patients and the overall healthcare experience.
The beauty of telehealth is that it provides access to a qualified provider at any time. For example, we have a client providing psychiatric services across the country. On a busy day, a patient presented that she was experiencing domestic violence trauma and that she was uncomfortable talking to a male doctor.
The problem is that there are only male psychiatrists on duty at her current hospital. The hospital contacted our team, and in turn, we contacted two privileged and certified female providers who were not available that day.
Although one was about to go to a wedding, she took up the task of taking care of this patient immediately. So even though this psychiatrist works five states away from hospitals, she is still able to provide care thanks to her ability to access healthcare remotely.
Result: The patient received the “right care” she needed at the right time with an experienced provider.
Follow Bill’s HIT coverage on LinkedIn: Bill Siwicki
Email the writer: [email protected]
Healthcare IT News is a publication of HIMSS Media.