AAMC/HRSA data reveals shortage of primary care, mental health physicians

The number of residents pursuing careers in primary health and mental health has increased in recent years, but there are still not enough specialists to meet current demand.
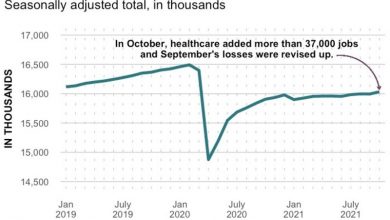
Labor shortages across the healthcare industry have resulted in delays in care and strained hospital resources. Hospitals and health systems as well as federal and state governments have tried to attract more people to the profession, but there is concern that the growing number of doctors entering the field will not be enough to meet the needs meet growing demand and a wave of retirees. .
There were 14,193 residents—a 15% increase over the past three years—trained in family medicine programs accredited by the Accreditation Council for Graduate Medical Education in the 2021-22 school year, while the shortfall currently exceeds 17,000 primary care physicians across the U.S. health care professional service area, according to the Association of American Medical Colleges and the Service and Resource Administration. Medical resources. For the mental health workforce, there are 7,093 psychiatrists—a 21% increase over the past three years—compared to a shortfall of nearly 8,000 physicians today.
The mismatch between supply and demand is partly due to the large difference in wages. The median starting salary for primary care physicians and psychiatrists last year was about half of the median starting salary for surgeons, according to data from the doctor search firm Merritt Hawkins. orthopedic and interventional cardiologists.
“The way we pay doctors in this country is so different,” said David Auerbach, a health economist and senior director of research and cost trends at the Massachusetts Health Policy Committee. distinction between primary care and other specialties.
That disparity is acutely felt in rural areas, he said, where a third of all doctors per capita are in urban areas.
As long as other professional services are priced and reimbursed much higher, these biases will persist, said Ryan McBain, policy researcher at the nonprofit consultancy RAND Corp.
However, Auerbach and other researchers warn that the shortfall estimate does not affect nurses and physician assistants, two of the fastest-growing job fields in the healthcare sector. According to the Association of American Medical Colleges, the growth of these two professions, which often provide primary care and are taking on a larger role in health care delivery, will partially offset the estimated primary care physician shortage of 17,800 to 48,000 by 2034.
Even so, the shortage of doctors and nurses is creating a large backlog. For example, many health systems are treating mental health patients in their emergency departments for longer periods because their post-acute referral partners are incompetent.
“Today, we are in a situation where there is a waiting list for mental health facilities,” said Vasanta Pundarika, co-head of healthcare investment banking at Matrix Capital Markets Group. inpatient and outpatient. “Given the lack of mental health doctors and psychiatric residents, will that waiting list continue to grow?”
Hospitals and health systems as well as federal and state governments are offering incentives such as free or partial tuition reimbursement for physicians pursuing primary and health care. mental health in underserved areas. But those efforts have had limited effect, industry observers said.
The Health Resources and Services Administration has funded a variety of scholarships and career development programs that promote the health care workforce in rural areas. While those efforts have helped, the divide between the number of doctors per capita practicing in urban versus rural areas has increased over the past decade, Auerbach said.
“You can only do so much to get people where you want them to go,” he says.
Telehealth has filled a number of care gaps as specialists at the academic medical center guide procedures performed in rural hospitals. The $1.7 trillion overall bill passed at the end could be helpful, as the law has extended telehealth reimbursement waivers through 2024.
Expanding the number of vacancies at U.S. medical schools can also help, says Rand’s McBain, noting that the average acceptance rate is about 5%. “This means that the United States is turning down a lot of potential talent,” he said.