Debunking Some Misconceptions About Performance Improvement Technology


Revenue cycle management is a great place for operational improvement technologies. These technologies can leverage process and task mining to give leaders a holistic view of their team’s workflow.
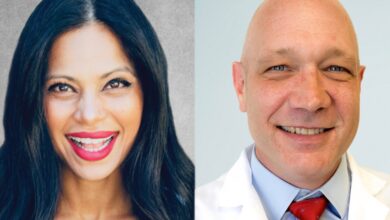
But according to Todd Doze, a 20-year healthcare industry veteran and CEO of Janus Health, a revenue cycle management technology company, there are three common misconceptions about operations improvement technology:
- Operational improvement systems replace human intervention – even though they are designed to help humans make better decisions.
- Operational improvement technologies lack the granularity needed to make decisions – although they provide detailed insights at the workflow level that the human eye cannot comprehend.
- Performance improvement systems require time that a team doesn’t have – though many organizations find these technologies help reallocate employees in a low-risk, high-reward way, allowing team members to work to their full potential.
Healthcare IT News sat down with tech CEO Doze to dig deeper into the myths he describes and the realities, according to him and his experience with technology, that he wishes more people understood.
Ask You say there are three common myths about performance improvement technology. Let’s dive into them. Your first myth: Performance improvement systems replace human intervention. Please explain why this is not true, in your opinion.
ONE. To fully explain this, let us start by outlining what operational improvement technology is. In essence, this technology is designed to help organizations get maximum returns with minimum effort.
It’s no secret that hospitals are understaffed, and not just on the clinician side. Back-office billing offices also face staff shortages and limited time in the day to process, track, and collect claims that overload their systems. These challenges, combined with difficult payer interactions, can make workflows extremely labor-intensive and inefficient, leading to delays. The most serious of these delays is late payments, which directly impact a hospital or health system’s bottom line.
The idea that performance improvement technology will remove human connection is flawed. In fact, the goal of this technology is to leverage processes and tasks to help humans make better decisions – not replace them.
One-third of healthcare overspending today is spent on administrative tasks, and those working in the billing/revenue cycle are no strangers to this dilemma. Technology that improves operations, often with the help of automation but not always, can provide data and contextual clues to help teams make the right next decision.
Sometimes that decision is knowing what and where to automate, and other times it’s realizing that processes need to be tweaked and employees need to be retrained to keep up. Change management is made possible by tools like this because it gets directly to the root of “how people work” and “what people do.”
You and your leadership team must decide what to do with those answers – decide how and what to optimize.
Q. Your second myth: Operational improvement technologies lack the granularity needed to make decisions. Why is this a myth?
ONE. While humans like to believe that we have it all figured out (and that nothing can get past us), the truth is that we all make mistakes in some form. For example, for years, health systems relied on internal process improvement teams or third-party consultants to examine workflows and identify areas for improvement.
Despite their best efforts, humans observing others at work is like looking through a limited lens. There are many reasons for this, the biggest being that individuals act differently when supervised. This compromises the understanding of the overall workflow, ultimately hindering optimization efforts.
The idea that an operations improvement system can provide insights into workflows that are beyond the human eye should be music to the ears of revenue cycle professionals. By focusing on the day-to-day workflows of individuals at the team, payer, or individual level, cracks in the foundation can be quickly identified and teams are better equipped to make course corrections when necessary.
For example, there may be an individual who is having difficulty resolving a claim. There may be a number of reasons for this, including but not limited to a combination of difficulty between payers, too many steps to take, not taking enough steps, etc.
The benefits of early detection of these issues will have many positive outcomes for the healthcare system or hospital, including: reducing inefficiencies leading to better performance, identifying broken or no longer serving processes for the organization, analyzing quality gaps that are costly in terms of time and money to maintain, and last but not least, preventing rejections.
H. And finally, your third misconception: Performance improvement systems require time that a team doesn’t have. Don’t they?
ONE. There’s no doubt that looking at the data that operational improvement technology can provide will take time and effort – like anything worth doing, it requires investment. However, I can confidently say that the potential for this time is negligible compared to the time your team is wasting on inefficient and outdated workflows.
If you’ve ever wondered, Is there a better way to expand our profit margins, or, What is my team really doing? then operational improvement technology is worth discussing.
In a recent AHA report, it was found that labor costs account for the largest portion of hospital costs. That’s a whopping $893 billion spent on labor, far exceeding other costs like medications and supplies.
Operations improvement technology provides a low-risk, high-reward way to ensure your workforce is performing at the highest level of their license. We all know the challenges that come with managing hourly workers, and it’s even more difficult when we don’t have a clear picture of how they spend their time.
Operational innovation technology eliminates guesswork and provides the level of security leaders need to manage their teams well.
Knowledge is power. Leaders owe it to themselves and their teams to have the right data to make decisions that are in everyone’s best interest. The sooner you can learn from that data and make decisions, the sooner you’ll free up more time – ultimately creating more profit margins at the business level.
Follow Bill’s HIT coverage on LinkedIn: Bill Siwicki
Email him: [email protected]
Healthcare IT News is a publication of HIMSS Media.