ATA Urges CMS to Enhance Telehealth and Issue Guidance ASAP
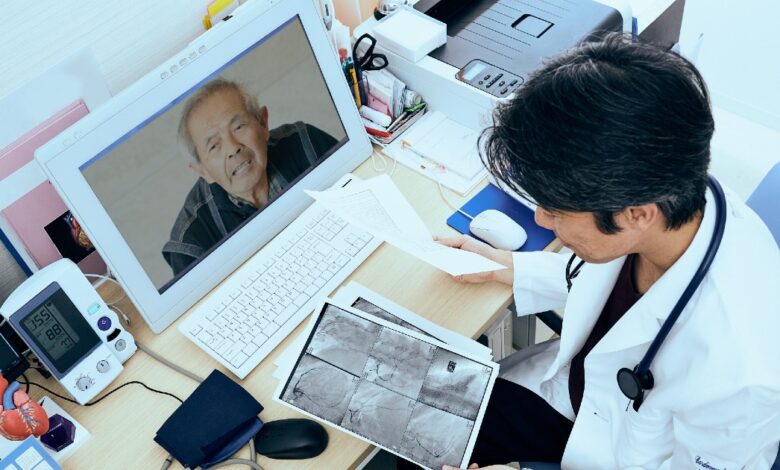

The American Telemedicine Association and ATA Action in a letter to the Centers for Medicare and Medicaid Services seek to maintain the flexibility of Medicare telehealth services during the pandemic, which they say is responsible for improving access to health care across the U.S.
The organizations said in a statement Wednesday that telehealth “plays a critical role in ensuring timely, appropriate, and expanded access to care for millions of Americans,” and that CMS should continue to engage stakeholders to ensure that services are covered and reimbursement rates for telehealth services are equitable.
WHY IT MATTERS
Without a legislative extension or change to the 2025 Physician Fee Schedule when it expires at the end of 2024, telehealth will essentially be relegated to limited service delivery to certain rural areas and specific locations, the organizations said.
“Without congressional action before the end of the year, we will not only be pulled back into how
“If we look at telecommunications in January 2020, we’re going back to 1997,” when federal lawmakers passed Section 1834(m) of the Social Security Act, Kyle Zebley, senior vice president, public policy at ATA and executive director of ATA Action, said in a statement.
“These outdated restrictions would erase more than half a decade of significant and meaningful progress, and reverting to these old restrictions would severely hamper access to telehealth services that millions of Americans currently use,” he explained.
Specifically, in a letter to CMS Administrator Chiquita Brooks-LaSure, telehealth organizations requested:
- Bypass geographical and origin restrictions.
- Maintain coverage for audio-only services.
- Allows reimbursement for telehealth visits to Federally Qualified Rural Health Clinics and Health Centers.
- Delay requesting a telepsychiatric visit before an in-person meeting.
- Maintain expansion of Medicare’s Telehealth Provider list to include physical therapy, occupational therapy, and speech therapy.
- Allows access to virtual cardiac and pulmonary rehabilitation services.
- Maintain the Emergency Care at Home Program.
- Allows virtual diabetes prevention platforms and supplies to participate in the Medicare Diabetes Prevention Program.
“We strongly believe that Congress will maintain Medicare telehealth flexibility beyond 2024,” the organizations said in their comment letter.
“As Congress formally enacts telehealth legislation, we urge the administration, in coordination with CMS, to promptly issue guidance to providers and others in the industry to eliminate confusion and ensure smooth implementation of telehealth regulatory policies beyond 2024.”
They also discussed several areas where they felt the agency fell short in strengthening telehealth services, including remote patient monitoring.
“We are deeply concerned that CMS has not addressed important issues raised by digital health stakeholders regarding the 16-day data reporting requirement for RPM billing and [remote therapeutic monitoring] codes, as well as other restrictive payment terms,” the organizations said.
While ATA and ATA Action called CMS’ recent addition of 13 new codes to Medicare Telehealth Services in its proposed fee schedule for 2025 “a step forward,” they asked the agency to make further additions to maintain “consistent and appropriate access” to essential patient care services.
For example, removing radiation treatment administration services from the Medicare Telehealth Services list “could inadvertently disrupt patient care and access to critical services,” ATA and ATA Action said.
THE BIGGER TREND
While CMS continues to add more reimbursement codes — such as cancer patient navigation services and dental care — to the physician fee schedule each year, provider groups were concerned when the 2024 Final Rule reduced their payments by 1.25% compared to 2023.
Health tech leaders see the reimbursement expansion in the 2023 schedule as a strong endorsement of telehealth innovation under Medicare.
This commitment provides the freedom to innovate and deliver better and more equitable care, said Dr. Robert Murry, medical director of NextGen Healthcare and a practicing family physician. Healthcare IT News at that time.
But by November, the agency’s cut in reimbursements had dampened provider enthusiasm.
Dr. Jesse Ehrenfeld, president of the American Medical Association, said in November that the Medicare physician payment schedule is “an unfortunate continuation of a two-decade journey that has made Medicare unsustainable for patients and physicians.”
ON THE RECORD
“We are concerned that reducing fee-for-service payment rates may inadvertently reduce incentives to adopt telehealth and hinder providers’ ability to adequately invest in the necessary technology infrastructure or incorporate it into their workflows,” ATA and ATA Action said in their commentary. “Payment equity should consider these various factors.”
Andrea Fox is senior editor of Healthcare IT News.
Email: [email protected]
Healthcare IT News is a publication of HIMSS Media.