US COVID cases start to rise again as holidays approach:


After falling for most of the fall, COVID-19 cases are on the rise again in many parts of the US
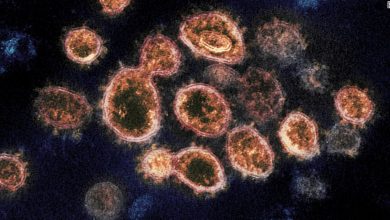
VALERIE MACON / AFP via Getty Images
hide captions
switch captions
VALERIE MACON / AFP via Getty Images

After falling for most of the fall, COVID-19 cases are on the rise again in many parts of the US
VALERIE MACON / AFP via Getty Images
It’s a worrisome sign for the US ahead of the holiday travel season: coronavirus infections are on the rise in more than half of the states. Experts warn this could be the start of a prolonged winter surge.
The increase is a change after cases fell steadily from mid-September to late October. The country now has an average of more than 83,000 cases per day – an increase of about 14% from a week ago and 12% from a week ago. with two weeks ago.
Dr. George Rutherford, an epidemiologist at the University of California, San Francisco.
Growing outbreaks in the Midwest and Northeast have largely driven the nation’s patient numbers, and that comes after weeks of high case numbers and strain in mountainous states West, where some hospitals are dealing with crisis levels of patients.
“There are still large swaths of the country unvaccinated, and even among states that are relatively well vaccinated, like Colorado, New Mexico, Minnesota and Vermont, we are seeing,” said Rutherford. sustained transmission.
The increase in cases has not yet translated into a nationwide spike in new hospital admissions, which tends to be followed by an increase in infections within weeks. However, the grim situation in some parts of the West and upper Midwest presents a worrying picture for other states, where cases are on the rise.
“This is a marathon,” said Dr. Kencee Graves at the University of Utah Hospital, in Salt Lake City, Utah, who describes her state, like much of the Mountain West, as being trapped in a “plateau of the rise” where diseases The hospital not only has an ICU full of COVID-19 patients, but many other types of patients that need care.
Despite the worrisome trends, the expectation among experts modeling the course of the pandemic is that an increase will not bring the same levels of death and severe illness as last year.
“The majority of the population has some form of immunity,” Nicholas Reich, a bioanalyst at UMass Amherst, who runs a predictive model for COVID-19. “That feels really different about this moment – there are fewer people to infect.”
How bad could it get?
The growth in cases was not unexpected, given the patchwork of COVID-19 immunity across the US, where about 60% of the population fully vaccinated.
Americans are moving around the same as they were before the pandemic, wearing masks less often than they did last year, people are spending more time indoors because of cooler weather and protection against the virus. Recurrent infections, including vaccinations and previous infections, are waning. Ali Mokdad, professor of Health Metric Science at the University of Washington Institute for Health Metrics and Evaluation.
“You put all this together – and what you see in Europe, where many countries with higher vaccination rates than the US are seeing an increase – it will, of course. out,” he said.
And unlike last year, the US faces a more contagious version of the virus that “makes it really hard to get rid of the chains of transmission,” not to mention “human nature is asking us to.” back before the Reich at UMass, Amherst said.
How bad the situation gets will come down to the complex dynamics around immunity. Southern states endured a ferocious wave over the summer, and that may have built enough immunity from the infection to protect them from another major outbreak this winter. Areas that have not faced similar increases, especially states in the northern half of the country, are now dealing with increases, but many also benefit from vaccination rates higher.
“The real question is how big is it going to be and is it really that significant? And my feeling is that in New England it’s going to hit a wall of vaccinated people,” Dr. Ashish Jha, Dean of the School of Public Health at Brown University.
“I think the Midwest and Great Plains – places that have lower vaccination rates but haven’t seen a big increase in the deltas – they are most likely to end up with a few infections in the next few days.” next week and month.”
Even with a small mutation, hospitals can still suffer
Even if hospitals have fewer COVID-19 patients overall, it’s clear that many are less prepared to deal with the demands of the pandemic than they were last year.
Dr Bruce Siegel, president of Essential Hospitals of America, which represents hundreds of public hospitals in the US, said: “Every hospital I spoke to in the last month has been severely understaffed, especially medical staff. dozen.
At the University of Utah Hospital, Dr. Graves said their spike ICU had to close because it couldn’t staff anymore, and last month patients had to wait an average of three to five hours for a bed. ICU. “Our resources and stamina are much worse now than they were a year ago,” she said.
In the Southwest, hospitals are also dealing with packed ICUs.
New Mexico has higher immunization rates than many neighboring states, but the state was forced to enact its crisis care plan standards a few weeks ago. Some hospitals have already activated those plans, but none have switched to the extreme scenario of deciding who gets care and who doesn’t, Troy Clark, president of the New Mexico Hospital Association.
Starting in the spring, there was a “large volume of patients that we don’t usually see” with other urgent medical needs, Clark said. That leaves hospitals extremely busy as winter approaches – and doesn’t have time to take on the growing number of COVID-19 patients.
It is a similar situation in many states, including Arizona, where the number of hospitalizations for COVID-19 is now as high as it has been since February. “We just don’t have more storage to increase COVID”, says Ann-Marie Alameddin, president of the Arizona Hospital and Healthcare Association.
The upper Midwest now has some of the highest number of cases per capita in the country. Minnesota hospital leaders advise people to exercise caution so that they do not require medical care for COVID or non-COVID emergencies. “This has never been more serious” speak Kelly Chandler of Itasca County Public Health, which includes the city of Grand Rapids, in a recent public statement. “We are at the crisis level of 2020, but without the same COVID precautions.”
As we head into the holiday season, the risk of COVID increases, with more people traveling and socializing indoors. But “we also have some things that are helping, like more vaccines and vaccinated children,” says Brown’s Ashish Jha. “So we’re at an impasse. I don’t expect us to have a terrible increase, but I can certainly imagine parts of the country seeing an increase in size. modest scale when people gather and when the weather is still cold.”
Rob Stein of NPR contributed to this report.