More Evidence Vitamin D Is Effective in Preventing COVID-19

Early on in the COVID-19 pandemic, it became apparent that vitamin D played an important role and could help reduce incidence of positive tests, infection severity and the risk of hospitalization and death.
The evidence of benefit was so clear, I published a scientific review1 in the journal Nutrients at the end of October 2020, co-written with William Grant, Ph.D., and Dr. Carol Wagner, both of whom are part of the GrassrootsHealth expert vitamin D panel.
This paper, “Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity” — which you can download and read for free — ended up being the second-most downloaded Nutrients paper in the 12 months following its publication.
The study with the most downloads that year and the all-time highest number of views (178,562) for any Nutrients paper was another vitamin D study2 by Bhattoa et.al., which found vitamin D supplementation reduced the risk of both influenza and COVID-19 infections and deaths. One of the coauthors of my paper, Grant, was a coauthor on this paper as well.
Several other vitamin D papers topped the lists of views, downloads and citations as well, which was a testament to the fact that many were in fact paying attention to the data rather than blindly believing media claims that there was “no scientific basis” for the recommendation of vitamin D for COVID.
More Evidence for Vitamin D
Since then, mounting data have continued to support and strengthen the recommendation of vitamin D against COVID. One of the most recent pieces of evidence is a paper3,4 that assessed the effectiveness of vitamin D supplementation for the prevention of COVID-19 in frontline health care workers, published in the June 2022 issue of Archives of Medical Research.
A total of 321 health care workers in four Mexican hospitals were enrolled, all of whom tested negative for COVID at the start of the study. They were then randomly assigned to receive 4,000 international units (IUs) of vitamin D per day for 30 days, or a placebo. Along with Real-Time PCR testing, participants’ vitamin D levels and antibody levels were also measured at baseline and again on day 45.
Follow-up was completed by 192 participants: 94 in the treatment group and 98 controls, and the difference in infection rates was pretty impressive. Only 6.4% of those taking vitamin D tested positive for COVID during the trial, compared to 24.5% of controls. (The p-value was less than 0.001, and anything below 0.05 is considered statistically significant.)
The researchers concluded that lower infection risk was associated with an incremental increase in the blood level of vitamin D, independently of vitamin D deficiency. This means, even if an individual started out with deficiency and still had a deficient or insufficient blood level of vitamin D at the end of the study, as long as it went up a little bit, it had a protective effect.
Shortcomings of This Study
As I’ve mentioned in most all previous vitamin D articles, for optimal benefit, it’s really your blood level that counts, not the dose of vitamin D used. Data from GrassrootsHealth’s D*Action studies suggest the optimal level for disease prevention and good health is between 60 ng/mL and 80 ng/mL, while the cutoff for sufficiency appears to be around 40 ng/mL.
In Europe, the measurements you’re looking for are 150 to 200 nmol/L and 100 nmol/L respectively. To convert ng/mL into the European measurement (nmol/L), simply multiply the ng/mL measurement by 2.5. It’s also worth noting that 4,000 IUs is a fairly low dose. If you’re deficient, you may need a whole lot more, perhaps 8,000 to 10,000 IUs a day, to reach an ideal vitamin D blood level.
The fact that they used fixed dosing and didn’t titrate doses based on vitamin D levels in the blood is a shortcoming of this study. To their credit, they did include vitamin D testing, even if it wasn’t the primary consideration. Ideally, a study of this kind would focus on getting the treatment group into a protective vitamin D level of 60 to 80 ng/ml, and then compare the effects with controls.
All of that said, this double-blind, randomized, controlled trial (RCT) was not available when I wrote my paper, and it’s good to know there’s now additional support for supplementation, even at relatively low, fixed doses.
Of course, sun exposure is exponentially superior to oral supplementation, and the only way to ensure you’re getting an ideal amount of sun exposure is by getting your vitamin D level tested on a regular basis (ideally twice a year, in winter and summer).
Why Sun Exposure Is the Best Way to Optimize Vitamin D
Why use sun exposure rather than oral vitamin D? The short answer is that sun exposure gives you far more bang for your buck. Not only is it free, but it also provides a plethora of biological health benefits over and beyond vitamin D production.
If the science of sun exposure interests you, check out Dr. Roger Seheult’s MedCram lecture above. In it, he explains the ins and outs of how sunlight impacts your health. One really important health benefit you can only get from sunlight and not oral supplementation is mitochondrial melatonin production.
The best review of the sun’s effect on melatonin is the February 2020 paper,5 “Melatonin in Mitochondria: Mitigating Clear and Present Dangers,” published in the Physiology journal. It’s written by the best researcher in melatonin, Russel Reiter, Ph.D., whom I first heard lecture on melatonin over 25 years ago.
Reiter’s key finding is that 95% of the melatonin your body produces is made inside your mitochondria in response to near-infrared radiation from the sun or other near IR sources.
Only 5% of melatonin is produced in your pineal gland. Melatonin is a master hormone,6 a potent antioxidant7 and antioxidant recycler,8 and a master regulator of inflammation and cell death.9 These functions are part of what makes melatonin such an important anticancer molecule.10
So, to produce melatonin inside your mitochondria actually makes perfect sense, as your mitochondria desperately need protection from the damage caused by oxidative stress produced in the electron transport chain.
In summary, your mitochondria produce ATP, the energy currency of your cells. A byproduct of this ATP production is reactive oxidative species (ROS), which are responsible for oxidative stress. Excessive amounts of ROS will damage your mitochondria, contributing to suboptimal health, inflammation and chronic health conditions such as diabetes, obesity and thrombosis (blood clots).
The good news is your body has a built-in way to counteract these ROS. Inside your mitochondria, you also have an antioxidant system, and the main antioxidant is melatonin. Melatonin also upregulates your glutathione pathway, which is another potent antioxidant pathway. So, your body is literally designed to address the destructive impact of energy production, but you need sun exposure in order for that mechanism to work.
Sun Exposure and the Prevention of Viral Infections
Interestingly enough, melatonin has also been shown to be an important part of COVID treatment, reducing incidence of thrombosis and sepsis11 and lowering mortality.12,13
Evidence suggests sun exposure may help combat any number of respiratory infections, including COVID, and the production of melatonin in your mitochondria appears to be a key part of how and why that works.
There are a number of observations showing COVID rates across the world correlate to the solar index or the amount of sun striking the area. Positive case rates also correlate with vitamin D levels in the blood. Higher blood levels correlate with lower incidence of COVID and higher rates of survival for inpatients.
The same correlation does not always appear when using oral supplementation, however. Here, studies have produced mixed results. Some studies looking at the effect of giving vitamin D to patients with severe COVID, for example, found no benefit, even at very high doses. So, what’s going on?
In short, your vitamin D level may simply be a marker for sun exposure. Many of the benefits of sun exposure may actually be due to factors that are unrelated to vitamin D. For example, research14 looking at UVA levels and COVID mortality rates found areas of the U.S., the U.K. and Italy with higher UVA also had lower COVID mortality rates.
Vitamin D does not rise in response to UVA, only UVB, so, something in the sunlight other than vitamin D must be responsible for the beneficial impact. In that particular study, they speculated that nitric oxide, which is produced in response to UVA, could be the key, as nitric oxide has been shown to limit SARS-CoV-2 replication in vitro.
But while it’s true that nitric oxide rises in response to sunlight (specifically UVA and near-infrared), the primary mechanism at work may in fact be melatonin, because it’s produced in response to the infrared spectrum — which makes up a much greater portion of the solar spectrum than ultraviolet — and works regardless of the angle at which it hits the earth.
Hence the southern part of England can have lower COVID deaths than the northern part, even though the entire country is too far north for vitamin D production.
Melatonin and Sunlight Are Intimately Connected
Melatonin and sunlight are intimately linked and their relationship is unique in the fact that there are two forms of melatonin, circulatory and subcellular, or that produced by your pineal gland and secreted into the blood, and that produced by your mitochondria and used there locally.
Both appear to be controlled by either the absence of sunlight or the presence of sunlight. While circulatory melatonin may be the “hormone of darkness,” subcellular melatonin is the “hormone of daylight.”
Since the beginning of human history, people have lived and worked outdoors during the light of day, absorbing light energy from the sky. An average of 10 hours outdoors each day, 70 hours weekly, was common. Today, we spend an average of fewer than 30 minutes a day or a mere three hours per week in daylight, according to a study by Dr. Daniel Kripke, professor of psychiatry at UC San Diego.15
It is likely that near-infrared photons stimulate subcellular melatonin synthesis in your mitochondria through cyclic adenosine monophosphate (cAMP) or NF-kB activation, or alternatively by stimulating bone marrow stem cells.16
However, if you fail to expose your skin to sufficient near-infrared light from the sun, then your mitochondria will have seriously depleted melatonin levels that can’t be corrected through supplementation. This is why it is essential to get in the sun every day you can and have as much clothing removed as possible. This is the time of year where nearly everyone in the U.S. can do it. So, no excuses now, shoot for an hour a day in the sun.
Vitamin D Level Is Directly Correlated to COVID-19 Outcome
As mentioned, over the past two years, many published studies confirm the wisdom of using vitamin D against COVID and other respiratory infections, and while sun exposure is best, oral supplementation can still be beneficial.
According to a Spanish study17,18,19 published online October 27, 2020, in The Journal of Clinical Endocrinology & Metabolism, 82.2% of COVID-19 patients tested were found to be deficient in vitamin D, the medical term for which is 25-hydroxycholecalciferol (25OHD).
While this particular study failed to find a correlation between vitamin D levels and disease severity, other studies have shown patients with higher levels do tend to have milder disease. In fact, one such study20,21 found your risk of developing a severe case of, and dying from, COVID-19 is significantly lower once your vitamin D level gets above 30 ng/mL (75 nmol/L).
In the video above, Ivor Cummins, biochemist and chief program officer for Irish Heart Disease Awareness, reviews a number of studies showing how your vitamin D level can impact the outcomes from COVID-19.
One of the reasons why vitamin D is so important against COVID-19 has to do with its influence on T cell responses. Animal research22 published in 2014 explained how vitamin D receptor signals regulate T cell responses and therefore play an important role in your body’s defense against viral and bacterial infections.
As noted in that study, when vitamin D signaling is impaired, it significantly impacts the quantity, quality, breadth and location of CD8 T cell immunity, resulting in more severe viral and bacterial infections.
What’s more, according to a December 11, 2020, paper23 in the journal Vaccine: X, high-quality T cell response actually appears to be far more important than antibodies when it comes to providing protective immunity against SARS-CoV-2 specifically.
Epitopes associated with SARS-CoV-2 have been identified on CD4 and CD8 T-cells in the blood from patients who have successfully recovered from COVID-19, and according to the authors, these epitopes “are much less dominated by spike protein than in previous coronavirus infections.”24
Epitopes25 are sites on the virus that allow antibodies or cell receptors in your immune system to recognize it. This is why epitopes are also referred to as “antigenic determinants,” as they are the part that is recognized by an antibody, B-cell receptor or T-cell receptor.
Most antigens — substances that bind specifically to an antibody or a T-cell receptor — have several different epitopes, which allow it to be recognized by several different antibodies.
We May Be Seeing the Results of Pathogenic Priming
Importantly, some epitopes can cause autoimmunological pathogenic priming if you’ve been previously infected with SARS-CoV-2 or exposed via a COVID-19 vaccine.26
In other words, if you’ve had the infection once, and get reinfected (either by SARS-CoV-2 or a sufficiently similar coronavirus), the second bout has the potential to be more severe than the first. Similarly, if you get the COVID shot and are then infected with SARS-CoV-2, your infection could potentially be more severe than had you not gotten the shot.
We’re now also finding the COVID shot can make you more susceptible to repeated COVID reinfections, compared to people with natural immunity, and the more shots you get, the greater that risk.
COVID-19 is now actually more than twice as prevalent among the boosted, compared to those who quit after the initial series.27,28 Pfizer’s pediatric trial and Moderna’s adult trial29,30 also reveal the shots raise, rather than lower, the risk of reinfection31 (meaning catching COVID more than once). I review these and other evidences for this in “Why Three COVID Jabs Are Worse Than Two.”
How to Optimize Your Vitamin D
In closing, remember that the most crucial factor when it comes to vitamin D is your blood level, not the dose, as the dose you need is dependent on several individual factors, including your baseline blood level. Again, the level you’re shooting for is between 60 ng/mL and 80 ng/mL (150 nmol/L to 200 nmol/L).
I’ve published a comprehensive vitamin D report in which I detail vitamin D’s mechanisms of action and how to ensure optimal levels. I recommend downloading and sharing that report with everyone you know. A quick summary of the key steps is as follows:
1. First, measure your vitamin D level — One of the easiest and most cost-effective ways of measuring your vitamin D level is to participate in the GrassrootsHealth’s personalized nutrition project, which includes a vitamin D testing kit.
2. Once you know what your blood level is, you can assess the dose needed to maintain or improve your level. Your first and primary goal is to get in the sun for one hour a day close to solar noon with minimal clothes on as this will not only increase your vitamin D levels but your melatonin.
If you cannot get enough vitamin D from the sun (you can use the DMinder app32 to see how much vitamin D your body can make depending on your location and other individual factors), then you’ll need an oral supplement.
Ideally, take oral vitamin D3 together with magnesium and K2, as you need 244% more oral vitamin D if you’re not also taking magnesium and vitamin K2.33 What this means in practical terms is that if you take all three supplements in combination, you need far less oral vitamin D in order to achieve a healthy vitamin D level.
3. Assess your individualized vitamin D dosage — To do that, you can either use the chart below, or use GrassrootsHealth’s Vitamin D*calculator. (To convert ng/mL into the European measurement (nmol/L), simply multiply the ng/mL measurement by 2.5.) To calculate how much vitamin D you may be getting from regular sun exposure in addition to your supplemental intake, use the DMinder app.34
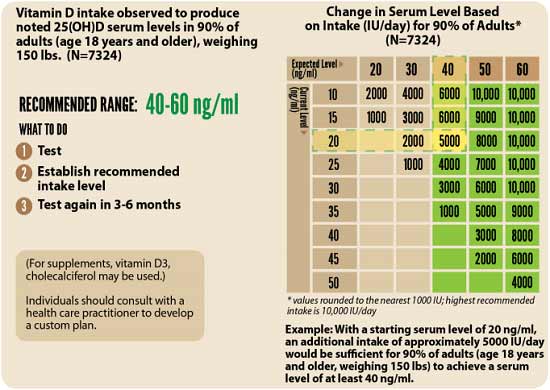
4. Retest in three to six months — Lastly, you’ll need to remeasure your vitamin D level in three to six months, to evaluate how your sun exposure and/or supplement dose is working for you.